Gated Access to Biomarker Testing
We all know that early detection of diseases is crucial for effective treatment and improved outcomes. But our current system often restricts the ability of doctors to order laboratory tests and biomarker testing unless patients present with symptoms or have an existing diagnosis.
It has become sick-care, not well-care, and certainly not proactive care.
Healthcare systems worldwide predominantly operate under a reactive model. Doctors typically order diagnostic tests only after a patient exhibits symptoms or has a medical history indicating the need for further investigation. Read that again: you can only get tests ordered once you’re already sick. You might not know you’re sick, but you could be sick.
This entire approach is rooted in the need to manage healthcare costs and avoid unnecessary testing for insurance companies. However, it also means that asymptomatic people may go undiagnosed for conditions that could have been detected early through routine screening.

Improve Health Outcomes with Early Detection
This is giving me a bit of PTSD from my Journalism degree and statistics classes, but it’s important stuff.
Numerous studies have shown that early detection significantly improves patient outcomes. For instance:
Cancer: The 5-year survival rate for localized cancer detected early is 89%, compared to just 21% for metastatic cancer. Proactive screening programs have been shown to reduce mortality rates in breast cancer and cervical cancer, up to 30%. According to the CDC, up to 25% of cancers in the U.S. are detected at an advanced stage, when the disease is more challenging to treat.
Cardiovascular Diseases: Early detection of high cholesterol and hypertension can reduce the risk of heart attack and stroke by up to 50%.
Diabetes: Early intervention in pre-diabetic individuals can prevent the progression to full-blown diabetes in up to 58% of cases.
Hypertension: Nearly 50% of individuals with hypertension are unaware of their condition because they have not been screened.

So Why Can’t People Get Their Own Biomarker Testing?
Several factors contribute to the current restrictions on ordering labs and biomarkers:

Proactive Testing
People are more aware of the benefits of proactive testing and are demanding access to the tests that give them insight into their health. It makes sense from a financial standpoint and from a humanity standpoint.
Biomarker testing gives people the ability to take preventative action. We can make lifestyle changes to alleviate, or even eradicate, conditions.
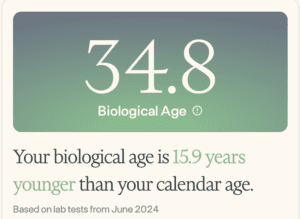
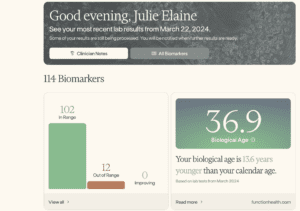
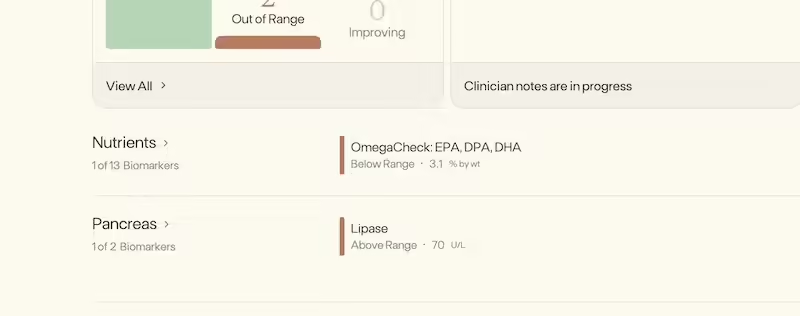
I have been regularly doing biomarker testing for the past 2 years, and it has provided me enormous ability to course-correct anything trending in an unhealthy direction.
Insights To Impact Epigenetic Change
Let’s get into 2 distinct use cases for biomarker testing, and two of the lifecycles my startup has particular focus on for now: preconception and perimenopause.
How Biomarker Testing Helps Fertility and Preconception
Biomarker testing can play a significant role in helping women with fertility by identifying potential issues early and guiding personalized treatment plans.
Some of the biomarkers you can look into include:

How Biomarker Testing Helps Perimenopause
Perimenopause, the often 10-year rollercoaster toward menopause, is characterized by fluctuating hormone levels that can lead to a variety of symptoms, such as hot flashes, mood swings, and irregular periods.
Biomarker testing can provide a clearer picture of what’s actually going on. For example, my biomarkers showed HIGH estrogen in my forties, not low estrogen. Many doctors simply looked at the age on my medical chart and made assumptions that were completely inaccurate.
Labs don’t lie—and they can and will validate your experience of feeling something is not right with your health.
Here are some of the things you can test for:

Biomarker Testing and Lifestyle Change
Importance of Personalized Nutritional and Lifestyle Plans
Based on biomarker testing, personalized plans can be developed to help people make targeted lifestyle changes that influence their epigenetics and alleviate or eradicate many conditions.
For women in transitional phases of life, biomarker testing is especially insightful. By understanding your hormone levels, inflammation markers, and epigenetic patterns, women can make informed lifestyle changes that improve their symptoms, improve their ability to conceive, and help balance hormones.
Proactive Testing is The Key
The restrictions on ordering labs and biomarkers only after symptoms arise have significant consequences for health.
Clearly, we require a movement toward more proactive testing, supported by statistical evidence and tailored guidelines. It can and will revolutionize the early detection and treatment of diseases, improving public health outcomes and reducing the overall burden on healthcare systems. It empowers and validates people with data that helps them make the steps to change their lives.
And…until it’s more readily accessible, you can work with a company like mine, Rêve Health. With us, you not only get access to all the tests needed to give you the full picture of insights, but you’ll also receive personalized guidance from a collective of holistic wellness experts, and community access helping you every step of the way on your wellness journey.