Western Healthcare Options For Fibroid Treatment
You Have Options For Fibroid Treatment
Do you have fibroids? Or suspect you have fibroids? Have you been told to “wait things out” until menopause?
By the age of 50, up to 80% of black women and up to 70% of white women have fibroids.
But at least 25% of fibroids cause symptoms so intense it affects our day-to-day lives. And…they don’t typically just stop growing. They get bigger and bigger, and their increased size equates to increased symptoms.
Symptoms of fibroids include weight gain, pelvic fullness, issues with bladder control, pain, issues conceiving, and heavy bleeding (I called my periods “crime scenes”).
For years I suffered from heavy periods, weight gain, hair loss on my scalp, hair growth on my face, brittle nails, and mood swings. Doctors told me nothing was wrong. It turns out I had fibroids.
As I sit here today writing this blog, I am symptom-free, with “normal” periods and no perimenopause symptoms. More important, I have no fibroids. Woohoo!
There are options to remove fibroids and live a vibrant life! I wish I had known about these when I first experienced symptoms.
Cure For Fibroids
Before I wrote this article, I searched “Cure for fibroids.” The first result said only a hysterectomy can cure fibroids! If a woman no longer has a uterus, there is no home for uterine fibroids. While technically it’s true that the end-all cure for fibroids is a hysterectomy, there are other options to remove fibroids.
According to a 2021 study, hysterectomy has been “the treatment of choice. Today, however, we have medical options that ameliorate these symptoms and reduce the size of the UF [uterine fibroids].”
Without further ado, here’s my list of western-medicine fibroid treatments.
As with any treatment, be sure to speak with your healthcare professional first. While I am not a healthcare professional, I am a trained journalist and a woman who explored all these options when dealing with my problematic fibroids.

Thermal Ablation
Fibroid Ablation
MRI-Guided Focused Ultrasound
Stanford Medicine describes MRI-guided focused ultrasound (MRgFUS) surgery as “High intensity focused ultrasound (HIFU) pinpoints a small target and provides a therapeutic effect by raising the temperature high enough to destroy the target with no damage to surrounding tissue. Magnetic resonance imaging (MRI) is used to guide and control the treatment, which is performed while you lie in an MR scanner.” This is a non-invasive fibroid treatment (no surgery, no cutting), and destroys the lining of the uterus. By integrating the thermal ablation with the precision of MRI-guidance, this can be a safe treatment option for women wanting to avoid surgery.
Radiofrequency Ablation
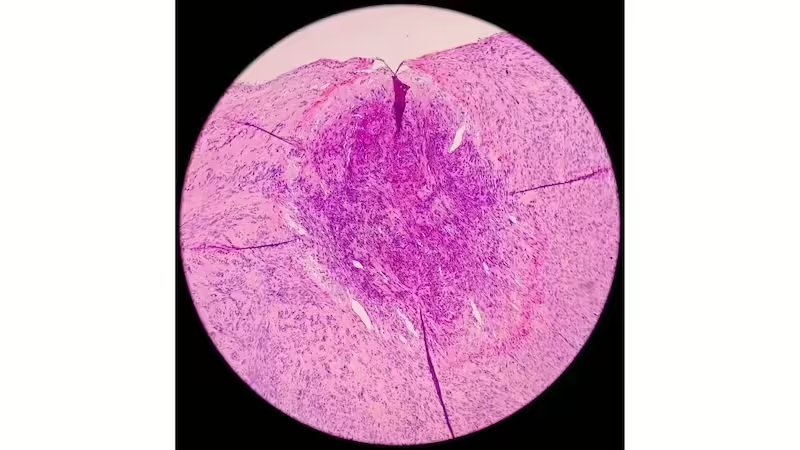
Radiofrequency ablation, such as Sonata, the Acessa procedure, or Lap-RFA, uses heat to minimize the size of fibroids. This procedure can be done through your vagina, through your cervix, or through a laparoscopy which means small cuts made in your abdominal area (sometimes through your belly button). According to the Mayo Clinic, the procedure uses a small camera called a laparoscope to find the fibroids; “After finding a fibroid, your doctor uses a device to send small needles into the fibroid. The needles heat up the fibroid tissue and destroy it. The destroyed fibroid changes right away. For instance, it goes from being hard like a golf ball to being soft like a marshmallow. During the next 3 to 12 months, the fibroid continues to shrink, and symptoms get better.”
More on the Sonata Treatment
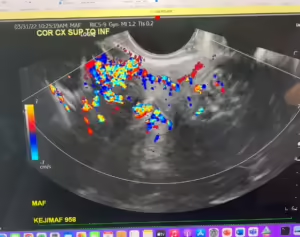
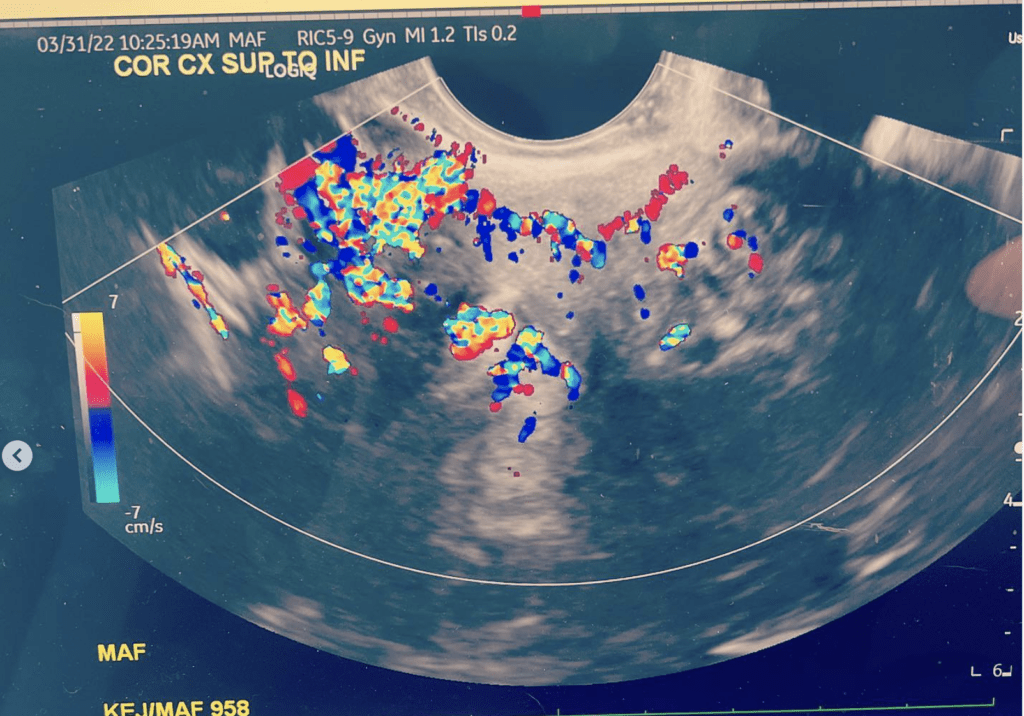
I personally explored the Sonata treatment at Brigham Faulkner hospital, and was shown what the handheld ultrasound tool looks like. It’s a small handpiece with an ultrasound tip that allows a doctor to go through the vagina and cervix (no surgery and no cutting) and uses radiofrequency to destroy fibroids. The procedure works best for smaller fibroids—in my case, because I had pedunculated fibroids growing outside the uterus, I was not a candidate.
The benefits to ablation include reduction of fibroid size and alleviation of associated symptoms without surgery (usually within 3-6 months, but check with your doctor). Your uterus and ovaries are not removed with this fibroid treatment.
Some of the cons include women experience pain from feeling the fibroids shrink. Some women unfortunately do not receive results from one treatment and need to undergo several treatments. I also personally did not like that I needed to possibly take GnRH agonists (Gonadotropin-releasing hormone), which help decrease the size of fibroids prior to the treatment (note here that I was able to reduce the size of my fibroids with acupuncture, which I’ll write another blog about).
Uterine Artery Embolization/ Uterine Fibroid Embolization
Uterine Fibroid Embolization (UFE) shrinks fibroids by blocking off their blood supply. Small plastic beads are injected into the arteries that supply the blood to the fibroids. These beads block the artery—they never move or migrate—and prevent the fibroids from “feeding.” The fibroids then shrink and dissolve.
The pros of this treatment include keeping your uterus and ovaries, no cutting, and a faster recovery time compared to surgeries.
The cons include possible fertility issues and an unsuccessful treatment where the fibroids do not shrink.
I personally rejected this option because studies have shown the beads can potentially block blood supply to your ovaries, and I did not like the idea of plastic beads forever being in my body.
A 2006 study showed “major complications include but are not limited to pulmonary embolus, uterine ischemia, necrosis, sepsis, and death. Non-life-threatening complications include altered ovarian and sexual function, subcutaneous tissue necrosis, expulsion of fibroid tissue, and treatment failure.”
Myomectomy Surgery (Fibroid Surgery)
There is a type of surgery specifically to remove fibroids while keeping your uterus called a myomectomy (which means removal of a myoma, another word for fibroid). While there is a technically a chance more fibroids could grow, it’s not as likely as doctors will have you believe, especially if you change the environment the fibroids grew in the first place (with lifestyle changes and other treatments).
I personally chose to have 2 myomectomies (one was an urgent surgery, and the second was a larger surgery after I had exhausted all other options) in order to avoid a hysterectomy. You can read more about this choice in my blog on gaslighting.
I’ll write another blog about how to help prevent uterine fibroids from coming back–which CAN occur after myomectomy if you do not address the reasons they grew in the first place.
In the meantime, if you want to “cut out” your problematic fibroids without removing your uterus, there are 3 types of myomectomy surgeries available. The size, location, and type of your fibroids will determine what kind of surgery is recommended.
Laparoscopic or Robotic Myomectomy
In a Laparoscopic myomectomy, your surgeon places small cuts in your abdomen and uses a tool (or tools) with a camera to find and remove the fibroids. Even larger fibroids can be removed this way with a procedure called morcellation, which cuts up the fibroid into smaller bits. A surgical bag is placed under the fibroid prior to the procedure to lower the risk of fibroid bits spreading through the body.
The pros of this surgery are you keep your uterus and ovaries, and because very small incisions are made in your abdomen there is less chance of infection. Your recovery time may vary between 2-4 weeks (ask your healthcare provider for more details).
According to Johns Hopkins, risks of robotic-assisted myomectomy include:
–Infection
–Excess bleeding
–Blood clots that can travel to the lungs and cause breathing problems
–Injury to nearby organs such as the bowel or ureters
–Wound healing problems
–Pelvic infection
–Pregnancy complications
–Reaction to anesthesia
–Regrowth of the fibroids after surgery
Hysteroscopic Myomectomy
If fibroids are smaller and inside the uterus, it’s possible to have a surgery where tools are placed through the vagina and cervix with no incisions outside the body or on the abdomen. Known as a hysteroscopic myomectomy, it is considered minimally evasive and typically performed without any damage to surrounding tissue.
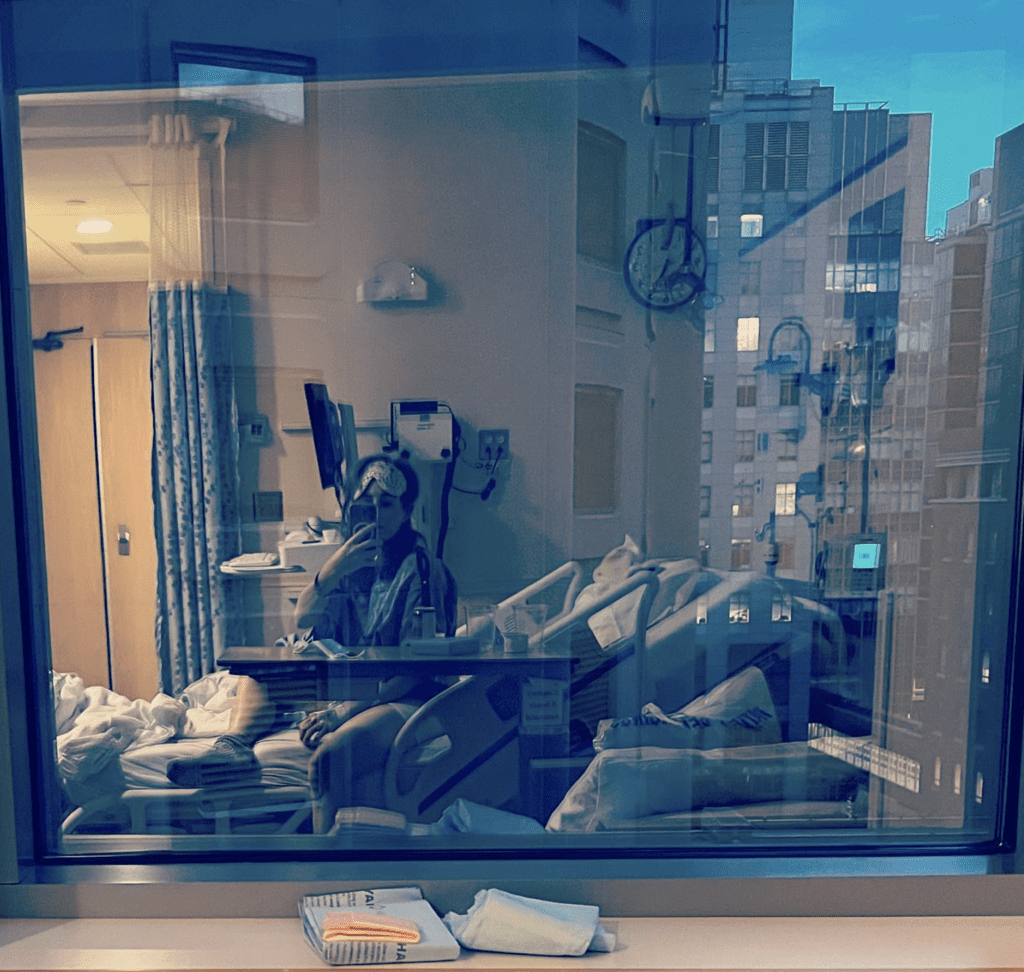
I had an urgent hysteroscopic myomectomy for just one fibroid which had detached itself from my uterine wall and was birthing itself (causing me to hemorrhage). It was a relatively quick surgery—a few hours for me—and while I did go under general anesthesia, my recovery was about 7 days. I took this option to give myself some time to figure out what to do about larger fibroids. This was how I personally avoided a hysterectomy–which for me was not an ideal solution.
The pros include NO cutting outside the body, a faster recovery time, keeping your uterus and ovaries.
According to Johns Hopkins; “Hysteroscopy is considered a safe procedure. As with any surgery, complications can occur. With hysteroscopy, complications occur in less than 1% of cases and can include:
–Infection.
–Heavy bleeding.
–Intrauterine scarring.
–Reaction to the anesthesia.
–Injury to your cervix, uterus, bowel, or bladder.
Reaction to the substance used to expand your uterus.”

Abdominal Myomectomy
This surgery may be right for you if you have large fibroids, or many fibroids, or if you want to ensure every part of your fibroids are removed. If you’ve been told your only option is a hysterectomy, you may want to seek a second opinion from a surgeon who performs abdominal myomectomy.
This surgery involves a larger cut in your abdomen. According to UCSF health this is also known as an “open” myomectomy, an abdominal myomectomy is a major surgical procedure. It involves making an incision through the skin on the lower abdomen, known as a “bikini cut,” and removing the fibroids from the wall of the uterus. The uterine muscle is then sewn back together using several layers of stitches.”
The pros of this surgery include the ability to remove very large fibroids often without morcellation (where they are cut up). This surgery can remove many fibroids all at once.
There are cons to this surgery including a much larger incision, infection, and longer recovery time than with other options. According to the Mayo Clinic, “Many women with uterine leiomyomas already have low blood counts (anemia) due to heavy menstrual bleeding, so they’re at a higher risk of problems due to blood loss.”
Women are at risk for blood transfusions during this surgery, yet “studies suggest that there is less blood loss with hysterectomy than myomectomy for similarly sized uteruses.” 1
My Abdominal Myomectomy
Because I had a 15-centimeter fibroid still in my uterus after my urgent hysteroscopic myomectomy, I had an addominal myomectomy.
My abdominal myomectomy resulted in a similar scar like a C-section. My recovery was similar according to people I know who’ve had BOTH an abdominal myomectomy and a C-section. It took me about a month to walk my dog down busy streets in Boston, and about 7 weeks until I could hike again. I’ll write a longer blog about this recovery (tip: hold a pillow over your stomach if you must sneeze!).
Abdominal myomectomy served me well and within a few months I had totally normal periods, no more crime scenes, and lost 15 pounds.
I wish I hadn’t let the fibroids grow to the point I needed surgery, but surgery did work well for me, and I am happy I did not have a hysterectomy.
Hysterectomy
Hysterectomy: This surgery removes the uterus. Once your uterus is removed, uterine fibroids no longer have a place to grow. You may see an improvement in problematic symptoms such as heavy periods—and no periods at all, ever again–within a few months after the surgery.
The pros to this surgery include absolute relief from fibroids, and the end to your periods. Many women report feeling relieved after this surgery, with no more chronic pain, no more bulk feelings in the pelvis, and having more predictable moods (often related to being on HRT, or hormone replacement therapy).
I coach women about the side effects and risks of hysterectomies. When I was exploring my treatment options I discovered hysterectomy is the surgery of choice in midlife, and that 90% of them are not medically needed.
Some healthcare professionals make it seem like a minor surgery that will solve all perimenopause or menopausal issues. Hysterectomy is a major surgery that—even if you keep your ovaries—can bring on early menopause. You will most likely require HRT, hormone replacement therapy.
According to HERS foundation, side effects of hysterectomy include:
–Heart disease
–Loss of sexual desire, arousal, sensation, and uterine orgasm
–Weight gain
–Osteoporosis
–Bone, joint and muscle pain, and immobility
–Painful intercourse, vaginal damage
–Displacement of bladder, bowel, and other pelvic organs
–Urinary tract infections, frequency, incontinence
–Chronic constipation and digestive disorders
–Debilitating fatigue
–Loss of stamina
–Altered body odor
–Loss of short-term memory
–Blunting of emotions, personality changes, despondency, irritability, anger, reclusiveness, and suicidal thinking.
Talk with your healthcare provider about all your options.
No Reason To Suffer In Silence When Fibroid Treatments Exist
Be aware that any surgeries (including myomectomies) are a business. According to HERS Foundation, “Gynecologists, hospitals and drug companies make more than $17B dollars a year from the business of hysterectomy.”
I wish I had researched fibroid treatment as soon as I had symptoms such as heavy bleeding. Had I acted on alleviating my symptoms a decade ago I might not have needed to have any surgery—but I’m happy to have explored all the options we have and to help other women.
Remember, there are ways to prevent fibroids from becoming problematic in the first place, and ways to alleviate and even eradicate them with holistic treatments and lifestyle changes.
There is no reason to suffer in silence for ANY duration of time when there are options available to live a life without any fibroid symptoms.
Have you had fibroid treatment? Share your experience below!